
Advantage Premiums Reflect Networks
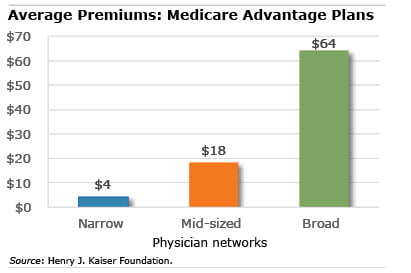
A new study of Medicare Advantage plans in 20 U.S. counties found that plans with higher premiums generally offer broader networks of physicians to their customers.
“There are exceptions but there does seem to be a fairly clear relationship between how much plans are charging and the size of the network,” said Tricia Neuman, a Kaiser senior vice president and one of the study’s authors.
The correlation between premiums and network size is one finding in a rare study that tries to get a handle on the quality of Advantage plans around the country amid a scarcity of data on these plans. An earlier Kaiser study looked at how many of a county’s hospitals and top cancer treatment centers are available in Advantage plans.
Advantage plans are increasingly popular for good reason: they have lower premiums or offer more extras than enrolling in the traditional fee-for-service Medicare program and purchasing a Medigap supplement and Part D prescription drug policy.
They are able to offer lower premiums based, to some extent, on their ability to keep their costs under control, whether this is how much they’re paying to their physicians or to testing labs. But because there is very little data on what Advantage plans pay for medical services, Neuman said that it’s difficult to sort out what is driving the plans’ costs – and, in turn, the premiums customers pay.
However, others argue that an insurer’s degree of control over the costs of its medical providers depends on how much market power it has over the physicians it pays for services. The federal Medicare program, for example, has tremendous clout to set prices for medical services, because it controls a large segment of the demand for health care by elderly beneficiaries relative to the supply of physicians and other medical service providers. Research suggests that Advantage plans may partly control their costs by anchoring their payments to Medicare’s payment rates. However, narrowing the networks may be another way for Advantage plan insurers to gain market clout to control costs.
There is wide variation, from county to county, in the breadth of the physician networks. For example, most of the retirees in Advantage plans in Clark County (surrounding Las Vegas) and in Harris County (Houston) are enrolled in narrow networks.
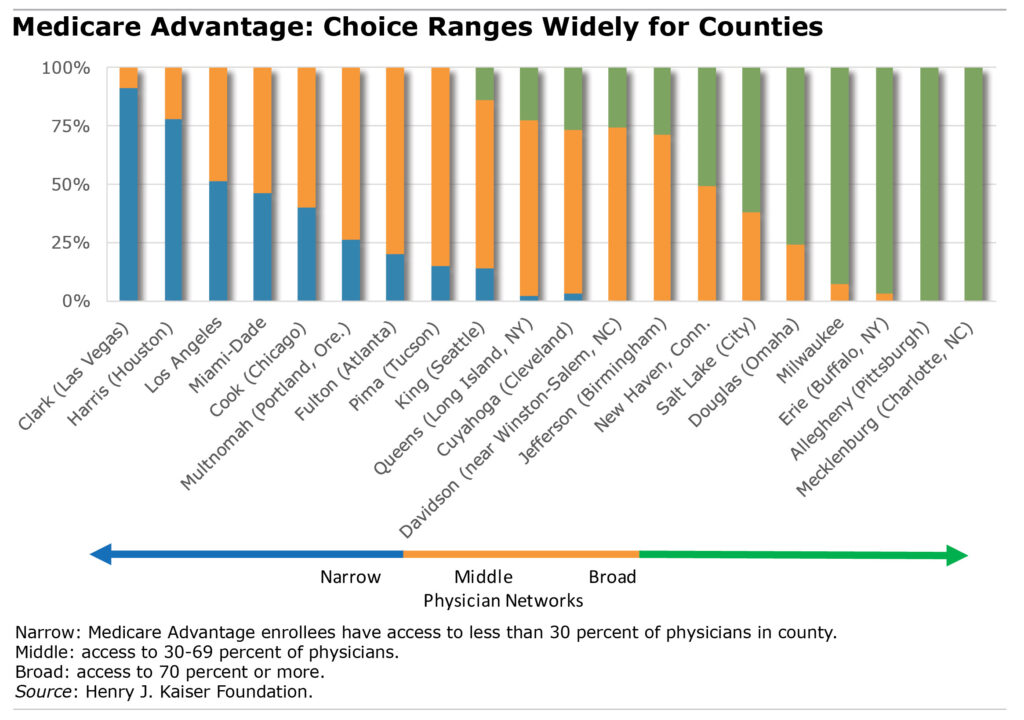
These counties contrast sharply with plans offered in Erie (Buffalo, NY), Allegheny (Pittsburgh), and Mecklenburg (Charlotte, NC), which included virtually all the physicians in their local areas. Premiums averaged $4 per month among the counties with narrow networks, compared with $64 per month where broad networks prevailed.
Medicare shoppers should keep in mind that Kaiser’s sorting of counties into narrow, mid-sized, and broad physician networks isn’t a definitive indication of the availability of physicians either, because some counties with narrow networks, like Los Angeles, have large numbers of physicians in their plans simply because they are very large counties. Further, even plans with large numbers of physicians may have much narrower networks of specialists. For example, Neuman said, 16 percent of the plans in Kaiser’s study used fewer than five radiation oncologists. This may not matter to healthy seniors shopping for a plan during the Oct. 15 through Dec. 7 open enrollment period but could become critical to those diagnosed with cancer.
The study also supported what many retirees already know: finding a specific set of doctors, especially in plans with narrow physician networks, can be extremely challenging. When the process frustrates retirees, they often take the easy route and stay with the same plan year after year, which can be more expensive than reconsidering the options every year.
Determining which doctors are in which plans isn’t easy either, in part because the Plan Finder on Medicare.gov does not list the physicians in each plan on offer during open enrollment period. To find doctors requires leaving Medicare’s website and searching through each insurer’s website for the plans under consideration.
“There’s no place where a consumer can ask which plans in my area include this particular doctor,” Neuman said.
And nearly half of the entries in physician directories contained inaccuracies, a study by the Centers for Medicare and Medicaid found earlier this year.
Advantage shoppers should take care.
Squared Away writer Kim Blanton invites you to follow us on Twitter @SquaredAwayBC. To stay current on our blog, please join our free email list. You’ll receive just one email each week – with links to the two new posts for that week – when you sign up here
Comments are closed.






What we are seeing the Baltimore-Washington market is a bit different. Here, several Advantage plans are organized around hospitals and health delivery organizations and their affiliated providers. These include MedStar Health (Georgetown Univ. Hospital), Johns Hopkins Medicare and the Univ. of MD Health Advantage program. These plans seek to get everyone’s interests in alignment, where they are the plan, the network, the hospitals and are their own insurance company.
Provider payments can be based on meeting certain metrics within their practices, as well as the plan meeting overall targets with incentives toward quality of care and not simply performing more services.
MedStar is shrinking it’s service area this year as Hopkins and U. of MD are expanding.
I would like to see Medicare step up and incorporate functional medicine doctors, chiropractic, and massage therapy into their programs — let’s start healing the causes and the “why” people are sick and stop treating symptoms by going to “specialists” where one doctor does not treat the whole person/body. Those specialists never talk to each other and we have a world filled with misdiagnosed and over prescribed human beings. A lot of these hospitals and doctors are surviving off kickbacks from pharmaceutical companies — a pill for your ill. I know too many people who are handed any type of medicine they “think” they need. It’s a messed up system indeed.