
Massachusetts Health Reform and the Labor Supply of Older Workers
Alicia H. Munnell is a columnist for MarketWatch and senior advisor of the Center for Retirement Research at Boston College.
Reform may prompt some workers to retire earlier.
A few weeks ago, I wrote about a brief we issued on the effects of Massachusetts’ health insurance reform. In addition to a literature review, the brief contained a new analysis of labor force participation for 55-64 year old males. No study had examined the labor market outcomes of older workers in Massachusetts, and these workers may be especially likely to be affected by health reform. In addition, researchers, including the Congressional Budget Office, have hypothesized that the Affordable Care Act (ACA) may reduce labor supply, either by making it easier to obtain health insurance outside of employers (through the exchanges or expanded public coverage) or because health reform alters the incentive to work.
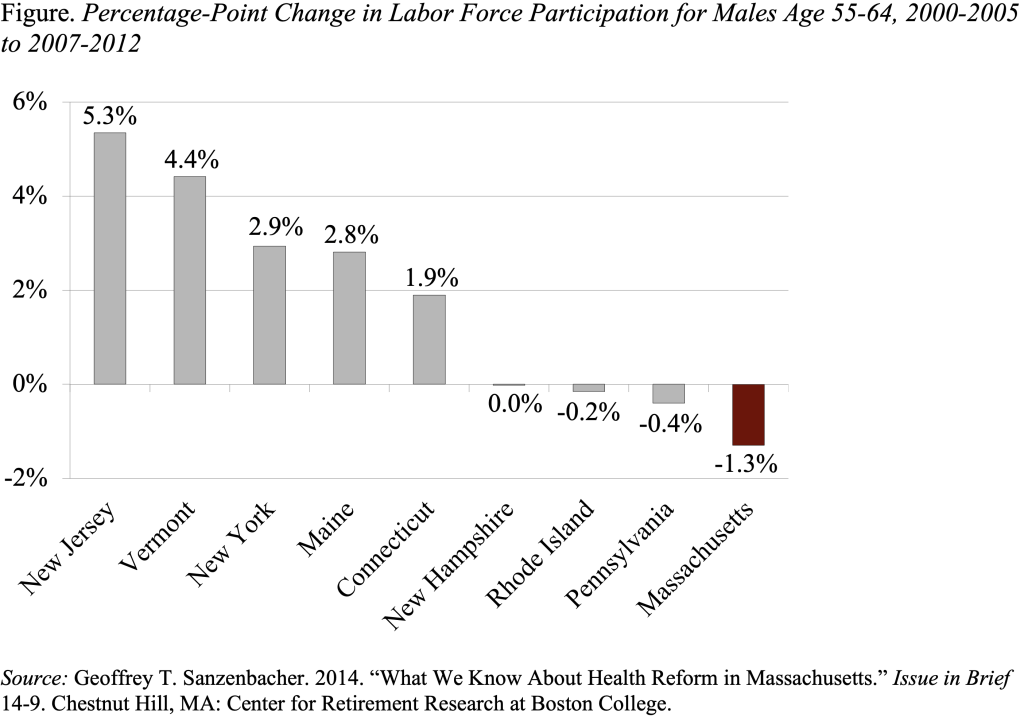
The analysis compared changes in labor force participation for Massachusetts before and after health reform to a set of nearby comparison states (the other New England states as well as New York, New Jersey, and Pennsylvania) over the same time period. The focus was on 55-64 year old males because females of this age group were less likely to participate in the labor force and more likely to depend on a spouse’s health insurance than males.
This analysis yielded an interesting result. It showed that, compared to nearby states, 55-64 year old males in Massachusetts experienced the largest decline in labor force participation between the time before and after the health insurance reform. Indeed, Massachusetts saw a decline in labor force participation among 55-64 year old males of 1.3 percentage points while the rest of the nation saw an increase of 1.7 percentage points. This result is consistent with research conducted by the Congressional Budget Office that shows health reform may reduce hours worked.
What explains this decline? Is it the ability to acquire affordable health insurance without having to wait for Medicare? One piece of evidence that would be consistent with such a story would be an increase in the percentage of Massachusetts men who are not participating in the labor force but have insurance. It turns out that prior to Massachusetts’ health reform, 93 percent of 55-64 year old males who were out of the labor force had health insurance; after the reform that number had risen to 97 percent. Most of this increase in coverage seems to have been through public health insurance programs.
The finding that older men in Massachusetts reduced their labor force participation more than those in surrounding states and more than the nation is of obvious interest to policymakers. If unhealthy workers – or people who simply hate their jobs – were able to leave the labor force because of expanded access to health insurance, economists argue that this reduction may not be a bad thing. (Although I do worry, since everybody does need to work longer in a world with increased retirement needs and reduced retirement resources, and waiting for Medicare has served as a disciplinary mechanism to keep people in the labor force.) On the other hand, if health reform alters the financial incentives to work through higher marginal income taxes on labor, as some have argued will be the case under the ACA, then a reduction in labor force participation may be a negative outcome of health reform. In either case, this analysis suggests it is worth keeping an eye on the labor force participation of older workers in the post-ACA world.







